
© 1997-2024 FNX Corporation and Trustees of Dartmouth College. All Rights Reserved.
CHAPTER 9: Pain
Contents
Up to one-quarter of adult patients are seriously bothered by pain. Pain often accompanies other problems. People with pain commonly report troubled sleep and limited ability to do physical exercises and daily activities. Pain is sometimes related to emotional problems. Please make sure your doctor understands the way your pain is affecting you and your confidence in managing and controlling other health problems.
What is Pain and Pain Management?
Types of Pain
Pain can be acute (new) such as that following an injury. Pain can be chronic (long standing) such as that resulting from "wear and tear" arthritis in a knee. Or it can be recurrent such as migraine headache that may come and go over many years.
Try to describe your pain well because understanding the type of pain can sometimes help you and your doctor find the best treatment. As examples, is the pain recurrent, chronic or acute. If it is stabbing, throbbing or pressure, it is most likely from skin, bone or muscles. If your pain is gnawing or cramping, it may be from deep in your body. If it is tingling, burning or shooting, it is probably from a nerve.
Typical Pain Management
Regardless of the acuteness or type of pain simple solutions should be tried first.
- Try local treatments for local pains.
Simple examples include getting wider shoes for sore feet or using ibuprofen or aspirin creams over a sore joint.
- Relaxation, music, or imagery.
Yes, these simple approaches do work for predictable pain. A simple relaxation approach requires that you turn on soft background music. (Without news or advertisements!) Lie down in bed or in a recliner, and let your jaw drop slightly, as though you were starting a small yawn. Keep your tongue resting on the bottom of your mouth. Let your lips get soft. Breathe slowly and evenly: inhale, exhale, rest. Allow yourself to stop forming words with your lips and thinking words. Think of pleasant pictures.
- Hot and cold.
Often warmth or cold over a painful area are effective. If warmth is chosen, be careful not to lie on a heating pad because it can damage your skin. Placing a damp cloth between your skin and the heat source provides moist heat.
- Aids and assistive devices.
For "wear and tear" arthritis or acute injury, canes, crutches and splints are often useful to reduce pain that bothers you most of the time and gets in the way of daily activities. But unless exercises are also used, an assistive device may make a person weaker and worsen the situation in the long run.
- Medicines.
First, try the safest pain medications first such as trisalicylate, salsalate, or acetaminophen. Pain medicines have to be tried for at least two weeks at an adequate dose before another is used. A medication that works wonders for one patient may have little effect in another. If the first medicines do not improve the pain, you have other choices that differ in cost and side effects. Most pain medications have a ceiling effect: you can take more and more pills and get no more pain relief.
Narcotics (like codeine) relieve many pains but have predictable problems: they may cause nausea, constipation, and drowsiness. They are also addictive; that is, you may need more and more to get the same level of pain relief. Low dose, long-acting narcotics can be very helpful.
- Special treatments for special pains.
Nerve Pains. Diabetes can cause nerve damage that usually affects the feet and legs, and sometimes the hands and arms. Nerve damage may cause numbness, tingling, burning, muscular weakness, or problems walking. People with this problem may be less aware of heat, cold, touch, and pain. Prevention by keeping the blood sugar as normal as possible is important because there are no medications that can reverse this process.
Another common cause for nerve pain is "shingles." This condition, caused by the chicken pox virus responds best if treated early with drugs called prednisone and acyclovir.
Inflammatory Pain such as rheumatoid arthritis: salsalate, aspirin, naproxen (Naprosyn), ibuprofen (Motrin), and many other similar medications called NSAIDs. Of the NSAIDS, salsalate and low-dose ibuprofen seem to have the lowest risk for causing stomach ulcers. For more severe inflammation prednisone and related steroids may be used for a short time only.
Chronic pain of unclear cause. Often the cause for long-lasting, chronic pain is not clear or several causes of pain may be present at once. When the precise cause of pain is unclear different approaches may be tested to see which one is most effective. The use of medication alone may not be practical or safe. For this reason chronic pain of unclear cause is a common reason for patients to seek help from chiropractic, acupuncture, herbal, nutritional, or massage treatments.
Common Causes for Pain in Adults
"Wear and tear" (Degenerative) Arthritis
"Wear and tear" arthritis is a common cause of long lasting, chronic and recurrent pain. the typical pain management approaches described above are usually effective. In particular, a pain diary often identifies the causes of the pain. Avoiding or changing certain activities may be very helpful for reducing pain.
Continued exercise is usually needed to avoid the muscle weakness that may worsen the arthritis or increase the risk for injury. For example,the knee gets most of its stability from the muscles around it. Knee stability depends less on the structures in the joint. Weight-moving exercise strengthens the muscles and can reduce wear and tear. Exercise also stretches the muscles. Please read Exercise and Eating Well for specific exercises.
Headaches
Migraine (vascular) headaches are often felt in the front and side of the head. They usually get very bad within 60 minutes and cause people to be sick to the stomach or want to avoid light. the headache is often pulsing or throbbing. There may be a twenty minute warning before the headache begins (for example, flashing spots, sick to the stomach). Alcohol, exercise, some foods (chocolate, preserved meats, and ice cream), changes in the weather, and the menstrual period may cause the headaches. The sufferer may relieve the headache somewhat by pressing on the arteries just above and in front of the ears. Migraine headaches come and go on their own and may last from a few hours to a day.
Muscle Contraction Type headaches usually begin gradually and get worse by the end of the day. The pain feels aching and pulling and is usually worse around the entire head and in the neck. The head may feel like it is being squeezed. These headaches may last for days or weeks. Exercise and hot showers may help a muscle contraction headache but make a migraine headache get worse.
Mixed headaches are a mixture of migraine and muscle contraction headaches.
The treatments for these three types of headache begin with avoidance of known causes usually identified by a pain diary. The next best approach is to use a safe treatment to try to reduce the headache. Aspirin, acetaminophen (Tylenol), ibuprofen, and naproxen are all effective medications that can be obtained without a prescription. Mixed and muscle contraction headaches are more difficult to treat with medicines alone. Therefore, many health professionals recommend a trial of relaxation, music, or imagery for these headaches when they are just starting.
To prevent migraine headaches, there are many prescription drugs: beta blockers, calcium blockers, anti-depressants; serotonin antagonists, and anticonvulsants. Riboflavin, a vitamin, also reduces the frequency of migraines. To treat severe migraine attacks, "triptans" have proved to be very effective.
Sinus headaches are another common headache. Usually it causes pains in the face that get worse when bent over. People may notice that they have a cold or runny nose when the have a sinus headache. Sinus headaches usually respond to nasal sprays or sinus/nasal decongestants for a few days (never more than 5 days). When sinus problems persist in a smoker, smoking is usually the cause. For non-smokers a one month trial of a cortisone nasal spray for several weeks may prove helpful.
Chest Pains
In young adults the cause of chest pain is usually not found. This pain is often sharp, brief, and brought on by exercise or made worse by deep breathing. Tenderness of the chest may be noticed also. These pains can happen a few times a day, or once or twice a week. Some people having asthma attacks can start with chest pain and shortness of breath as a first sign, rather than with coughing or wheezing. (See "Common Conditions").
Chest pain with shortness of breath or difficulty breathing is almost always of concern. A doctor should be contacted immediately when new or worsening chest pain with shortness of breath is noticed. Men having a "heart attack" often notice severe, squeezing pain with shortness of breath. A lung infection is another cause of pain and shortness of breath.
"Stomach" or Abdomen Pains
Pain in the abdomen can have many causes. New abdominal pain usually requires a visit to a doctor.
Pain in the abdomen that comes and goes over the years can be caused by several conditions. The most common conditions are due to the irritable bowel syndrome, peptic ulcers or dyspepsia (dis-pep-see-ya), and acid reflux.
Irritable bowel syndrome often causes discomfort around the belly button area. It can be quite severe at times and changes in bowel pattern may be noticed with it. For a day or two there may be diarrhea (lots of loose bowel movements) followed by constipation (can't go). Usually the discomfort lasts only for a few days but it can last for weeks.
Irritable bowels are usually managed by the addition of fiber to the diet -- unprocessed bran, vegetables, fruits, whole grain products -- and regular exercise. Avoidance of excessively fatty or gassy foods (beans, cabbage) may be helpful. Different medications may still be needed for persons bothered by pain (dicyclomine), diarrhea (loperamide), or constipation (lactulose). Peppermint oil is also often effective.
Lactose intolerance and celiac disease are less common than irritable bowel but very similar to it: both can cause the same type of discomfort and changes in bowel patterns. Lactose is a sugar in milk and milk products. About 15% of the white population and as high as 90% of African and Chinese Americans may have bloating, gas, and cramps when they have lactose. They can either avoid eating lactose or try lactase pills. However, many persons who have a normal ability to digest lactose also have these problems. Celiac disease is even less common than lactose intolerance. Celiac disease caused by the gluten contained in wheat and a few other grains.
Peptic ulcers and dyspepsia cause a burning or gnawing ache in the upper middle abdomen just below the chest. It is often most noticeable 1 - 4 hours after meals. Usually the pain is made better by eating meals or antacids. When the pain persists, an ulcer (an open sore in the lining of the stomach) may be present. Special tests may be done to see the ulcer with x-ray or a tube passed into the stomach. Persons with ulcers or dyspepsia who notice tar-like bowel movement (old blood) or persistent pain while being treated should contact their doctor immediately.
The most important treatment to help dyspepsia and ulcers is to avoid alcohol, aspirin, ibuprofen (and similar medications), coffee, and smoking. Persons who continue to smoke have great difficulty healing a peptic ulcer. When an ulcer is present, treatment may include antacids after meals, "stomach coating" pills (sucralfate), medications to cut down acid in the stomach (cimetidine, ranitidine, famotidine, omeprazole), and sometimes, antibacterial medications. With the exception of antibiotics, the treatments for dyspepsia are similar to those for peptic ulcers. When antacids are used they have to be used frequently: within 30 minutes of a meal and 1 and 3 hours after meals.
Acid reflux means that the "door" that normally keeps acid in the stomach allows some acid to leak back (reflux) into the swallowing tube (esophagus). The reflux causes pain or "burning" in the upper abdomen that is often made worse when the person lies flat or bend over. The pain is often worse after a big meal or within an hour after eating.
A key treatment is to raise the head of the bed by placing 6 inch blocks under the bedposts. Merely using pillows is not the way to keep acid in the stomach -- it often makes the problem worse. Using antacids and acid reducing pills is another treatment similar to that for dyspepsia and peptic ulcers. Certain foods should be avoided that allow the "door" to open: those high in fat or sugar -- particularly chocolate. Finally, weight loss in over-weight persons can really help take the pressure off the "door."
Low Back Pains
Many studies of back pain have been done and many treatments have been offered to sufferers. Out of all the studies, several patterns are clear: 1) almost all back pains get better over time. Few persons with back pain suffer disability -- even those who have a "slipped disc"; 2) x-ray or MRI results don't tell very much - persons with a lot of "wear and tear" on the xray or "disks" on an MRI may have no back problems whereas some with near normal x-rays may be bothered a lot.
Pain that increases when coughing or that goes into the legs suggests a "slipped disc" of the cushion between the bones of of the back. The disc will usually heal over time without causing problems. Rarely, a disc can squeeze out and pinch the nerves that go to the legs and bladder.
Treatments for new, low back pain, usually involves the use of mild pain pills (aspirin, acetaminophen, ibuprofen, etc.) and reducing activity briefly. When standing it is helpful to put one leg up on a footstool -- this will take pressure off the back. Several days of bed rest with stronger pain pills or sedatives may be needed when the pain is very severe. However, bed rest may actually slow down the speed of recovery, so excessive rest is best avoided. Applying heat or cold to the painful area and lying on the side or on the back with a pillow under the knees in bed sometimes helps.
About 80% of persons with new back pain who follow this approach will be able to return to normal activity in a week, although the average length of pain will be about two weeks.
For low back pain without pain going into the leg, chiropractic care may help some persons get better faster.
To avoid future problems the following seem to be useful: - Lifting correctly. Lifting is done with the legs by squatting with the back straight, knees bent, and weight held close to the body. Hand trucks or assistance is used for heavy weights. (More than 40 pounds for women and over 80 pounds for men). - Facing or holding the object to be lifted directly in front of the body. Avoid twisting the back, particularly when lifting or bending. - Sleeping on a very firm mattress or with a board under the mattress. - Keeping weight near the "ideal".
For chronic back pain and the avoidance of future back problems, exercise is very important. In fact, some studies suggest that intensive exercise is needed to reset the pain nerves so that they are less sensitive. A typical exercise is as follows: while lying on the floor, (with a small pillow under your head), bring your knees to your chest slowly, clasp your hands in front of your knees, pull them toward your chest and count up to ten. Relax, then repeat this three times and then relax with your knees bent, feet resting on the floor. Now tighten your abdomen and buttock muscles for ten seconds and you should feel your back flatten against the floor. Now repeat these three exercises again.
When back pain is so severe that everyday function is not possible or if the nerves are damaged (numbness or weakness), surgery or other back procedures may be needed to treat the damaged disc. Back surgery will make this severe problem get better quicker than waiting for the disc to heal on its own BUT over several years back pains may come back as often in people who have had surgery and those who have not had surgery.
Neck and Shoulder Aches
Neckaches and shoulder pains, like back pain, typically last for days or weeks. General principles of pain relief are the same. Plain x-rays add very little useful information.
Neck pains that should be evaluated by a doctor include:
- Neckaches that come on suddenly and have severe headache or fever.
- Neck pains that go into the arms.
- Neckaches and shoulder pains that do not increase with movement.
- Shoulder pain with fever, swelling, or redness.
Neckache
Self-treatment for neck pain includes gently stretching of the neck. The neck should not be "over bent" as for example, when using a big pillow. A soft collar can be worn around the neck to gently support and warm it until the problem gets better. (The "collar" can be made by taking a regular towel, folding it lengthwise in thirds, wrapping it around the neck and pinning it with a few safety pins). The collar should be worn round the clock if nighttime use alone is not enough does not relieve the pain.
Chiropractic treatment for neck pain, as with low back pain, may speed recovery in some patients.
Bursitis/Tendonitis
If the shoulder hurts when the arm is moved to comb hair the cause is usually "bursitis/tendonitis" of the shoulder.
When this problem comes on suddenly, the shoulder should be rested for 24 hours and use ice packs repeatedly for 30 minutes out of every 45-60 minutes for 12 of those 24 hours. After this rest period, mild exercise should be started. For example, "stretching" by resting the hand of your "good" arm on a countertop, bending at the hips, hanging your "bad" arm down. Slowly draw small circles with it. Gradually make the circles bigger but don't force it if it feels painful. Another exercise is to stand sideways about two feet from a wall so that you can reach it easily with your fingers. Now slowly use the fingers of your "bad arm" to "walk" your fingers up the wall. Stop when you start to feel pain. Do each of these exercises for about five minutes, twice a day.
Persistently reduced shoulder movement may benefit from an injection of cortisone and exercise; however, the shot may not do very much for pain. Sometimes "shockwave ultrasound" can be helpful. Finally, there are surgical options.
Pain Management in the Elderly
Aging changes the way pain should be managed because:
- Compared to younger persons, older persons are at increased risk to be over or under treated for pain.
- Older persons often have other conditions and reduced kidney and liver function. These differences place older persons at greater risk for medication problems.
- Commonly used mild pain relievers like aspirin, ibuprofen, and tylenol are more likely to cause stomach upset and kidney problems in older persons.
- Reactions like headache, worsening constipation, and thinking problems occur frequently from many types of pain medicines.
- Medicines for the anxiety, depression, and sleep disorders that may accompany pain can have additive side effects with the pain medications.
A Pain Diary and Pain Management Plan
For some people, pain can be a bothersome problem for a long time. Being able to successfully manage pain is a big help in being able to live well despite the problem of persistent pain. The Problem Solving tool in HowsYourHealth can automatically help people develop a PLAN for pain management. An example of a PLAN is shown below.
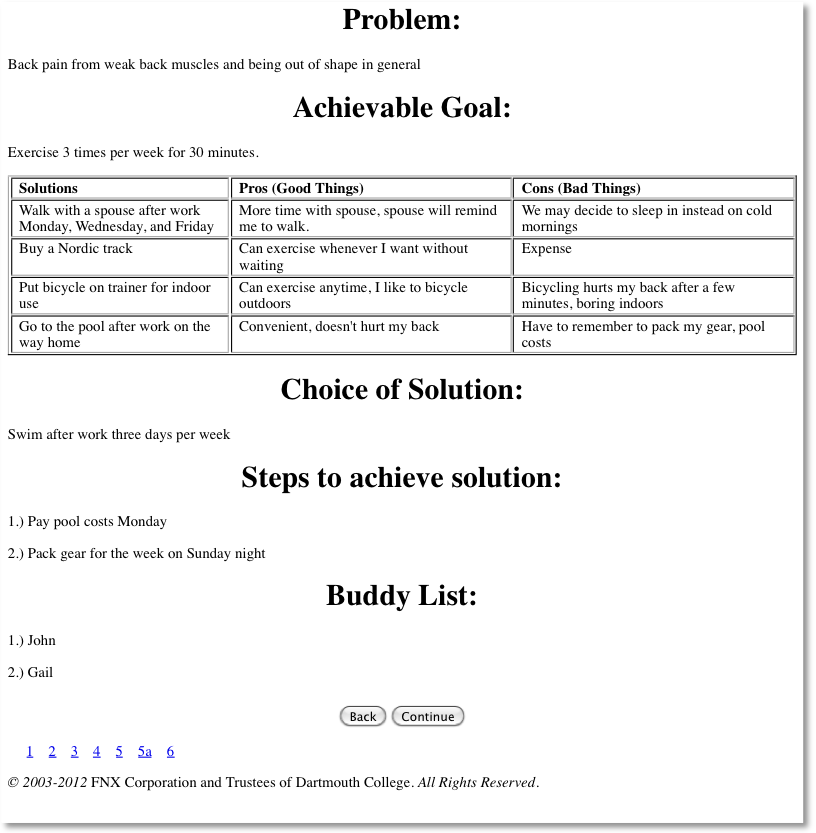
Once there is a plan for managing pain the PLAN should be tested. A DIARY is a very good tool to test the plan. Below is an example of a way to use a diary.
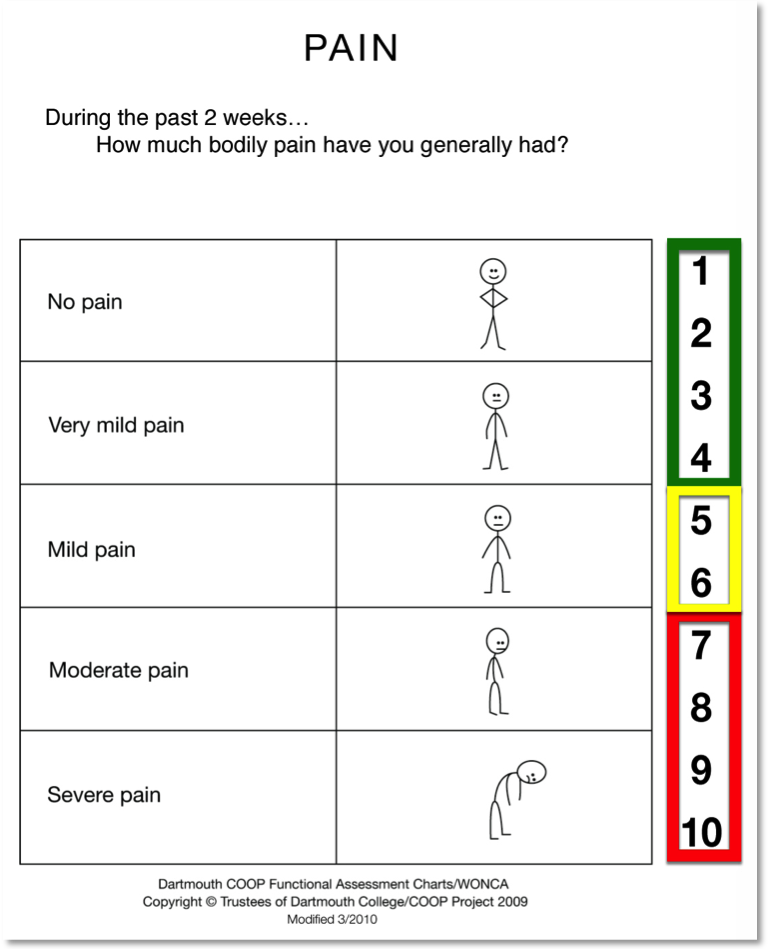
First, record your pain level using the Chart below. You may do that every day, every week or every two weeks.
Second, record what PLAN or treatment you are testing.
Third, record if the treatment is changing the pain by using the Chart.
Fourth, record any things you notice are worsening the pain.
Finally, with what you have learned go back to Problem Solving and build a better PLAN to test.
Pain Diary
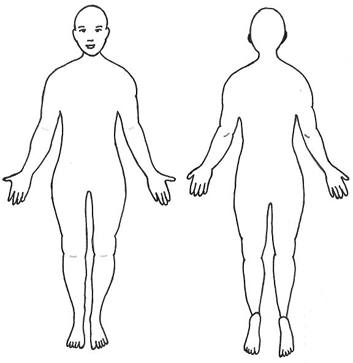
| Keep Track of Time: Day/Week | Record Pain Number From Chart | Location of Pain: Draw Diagram if Needed | Treatment or PLAN You are Using | Write here anythings that make the Pain Better or Worse |
Printable version of pain diary
To manage your pain, Go TO Problem Solving.
We have tried to make the How's Your Health error-free. However, those involved in its preparation can not warrant that all of the information is accurate and complete. When you use How's Your Health as a guide for your health and medical care, be sure to discuss any questions about it with your doctor, nurse, or other health care worker.
To choose another chapter, click the 'BACK' button.
Last reviewed: January 2024 © 1997-2024 FNX Corporation and Trustees of Dartmouth College. All Rights Reserved.